
Announcements of early coronavirus vaccine breakthroughs have inspired new hope this may be the beginning of the end of Covid-19. Developing a vaccine is one thing. How best to distribute a vaccine is a whole different question – with some difficult ethical questions.
The large scale distribution of a vaccine is an an incredible logistic task. Sure, things have become easier since the 19th century. Back then people transported a cowpox ‘vaccine’ over the Atlantic by creating a chain of 22 boys who were in turn infected with cowpox to keep the virus alive during the passage. But the task at hand is still immense. Pfizer’s vaccine candidate, for example, must be stored at around -70° Celsius and will therefore not be available in pharmacies any time soon.
But for now let’s assume we were really really good at figuring these things out. We have thousands of appropriately sized fridges, we have shipment containers and trucks in place. We built dedicated centers so people won’t have to wait in line and risk infecting each other waiting for a vaccine. Let’s assume we planned all these things months ago (of course we did, we are not stupid).
A moral choice
Now – whom should we give the vaccine to? The intuitive answer is of course: You give the vaccine to those that are most at risk, especially
- elderly people
- immuno-compromised individuals
- healthcare workers dealing with Covid-19 patients
Healthcare workers are most at risk of contracting the disease, while the elderly and immuno-compromised are most at risk of suffering heavily from the disease if they ever get it. Two different societal norms suggest this prioritization is the right one to make. On the one hand we have a strong norm to protect the most vulnerable among us – giving the vaccine first to those who would be most harmed by contracting the disease almost seems like a no-brainer. On the other hand our norms promote fairness: Those who risk their lives fighting the pandemic must be honored and protected as good as we can. This is what basic human decency demands.
To be precise, the criterion for whom to protect is not to prioritize those most at risk. It is instead to prioritize those who are at risk through no fault of their own.
Take healthcare workers. There are a lot of good arguments to be made that they should be among the first to be vaccinated. We need a functioning healthcare system to cope with the pandemic. Healthcare workers are among those most likely to encounter new cases and spread the disease into the community. But also, it is not their fault that healthcare workers are likely to contract and spread the disease. On the contrary, they are doing us a great service and we cannot demand of anyone to put themselves at risk without the best possible protection.
Now think of someone who has a similar epidemiological risk profile – but entirely because they choose to engage in risky behavior. Such a person is probably young, maybe male, likes to travel and to socialize with other people. They probably plays by the official rules, but might not be very cautious or afraid for themselves. As long as the lockdown is in place, they will probably stay at home, but once restrictions are eased, they is going to socialize as much as is permitted (and maybe even slightly more). Even if they follow the rules, there is quite a few social contacts they can have. Just like the spread of a virus, network sizes can grow exponentially – even if you only interact with a couple of people a day.
We, as a society, would regard that person much less favorably. Collectively, we would not like to give them special treatment. They chose to engage in risky behavior, putting themselves and others at risk. Most would say it doesn’t feel right to prioritize them when distributing a vaccine. But maybe we should do exactly that.
Fat tails in infectiousness
Instead of targeting the most vulnerable, we could target those who are most likely to spread the virus. Many suggested that Covid-19 infections follow the 80/20 rule: 80% of transmissions come from only 20% of infected individuals. Some suggest that around 70% of infected individuals don’t transmit the virus at all. I’m not too sure about the exact numbers, but it seems plausible that there is high variability in the number of people infected by different patients. Outbreaks are to a significant extent driven by superspreader events.
Let’s quickly look at superspreaders. Koen Swinkels and others have compiled a database with over 1 600 superspreading events (see here, here, and here). At the time of writing, 189 794 infections were recorded in the database. Let’s look at their distribution.
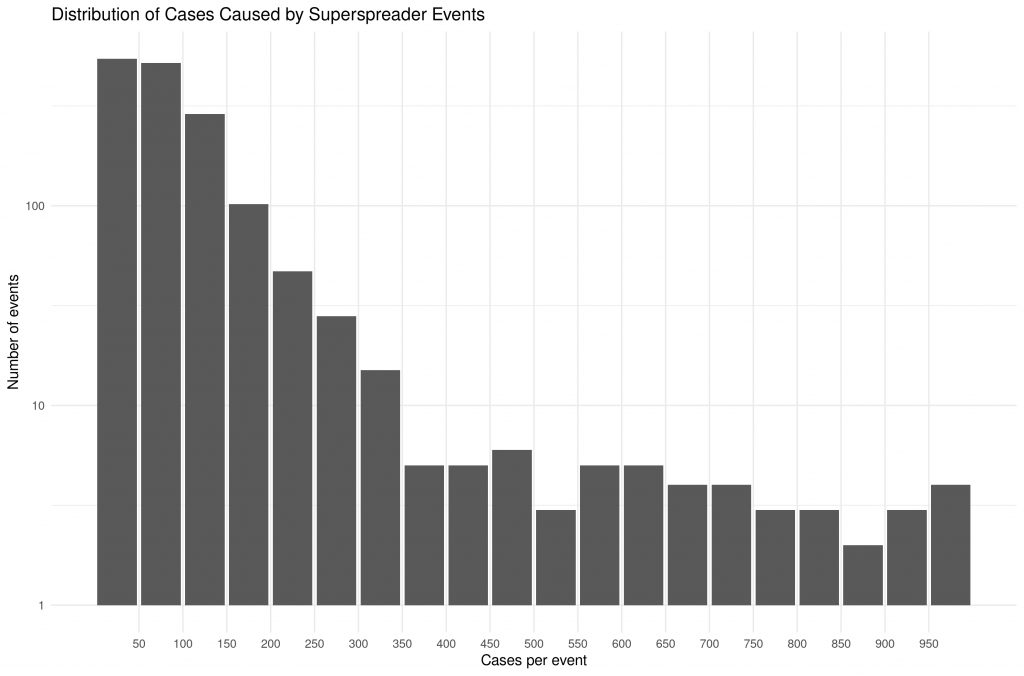
The median event had 78 cases, the mean had 118.2. Ten events had more than 1 000 cases (not shown in the plot) and the largest had 7 000. This data is of course incomplete. Not all superspreading events are included in the database. It does, however, give a sense of the magnitude of the problem. Preventing some of these events could go a long way in mitigating the pandemic.
Surely we could prevent these events by simply banning mass gatherings? Yes and no – let’s look at the settings in which these events happened:
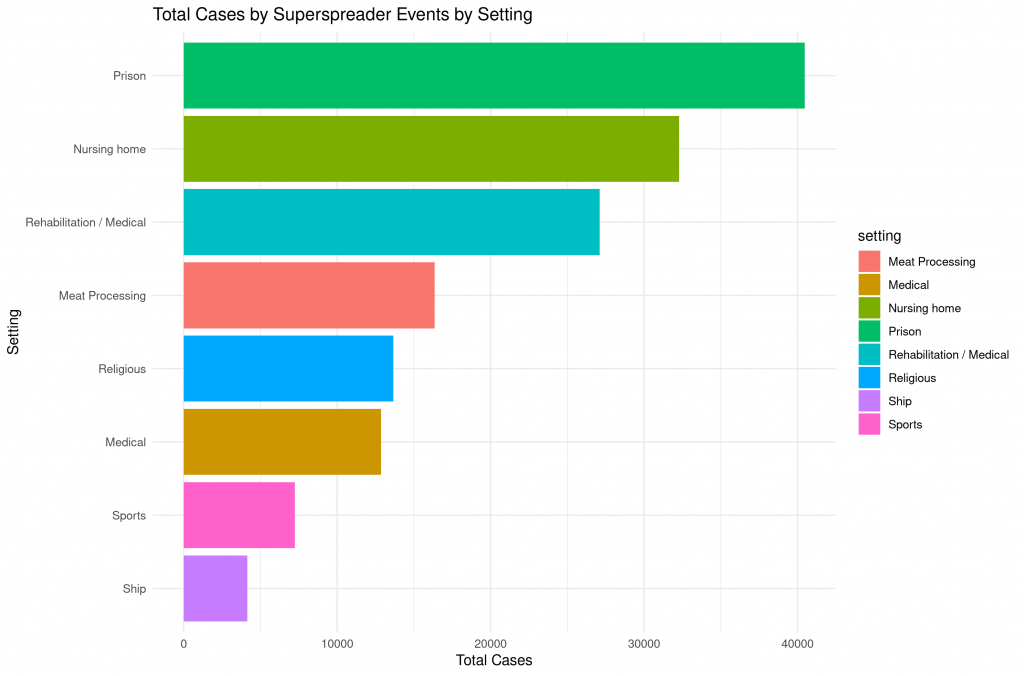
Some of the events were definitely preventable. Having mass sports events for example, is obviously just plain stupid. But the case is much different for everything related to healthcare or the prison system. I’m not sure you can simply shut down meat processing plants (I wish you could) and in many countries it is nigh impossible to ban religious gatherings.
While we’re at it, let’s look a little deeper at the setting and season of the superspreader events. Most events happened indoor and during the flu season:
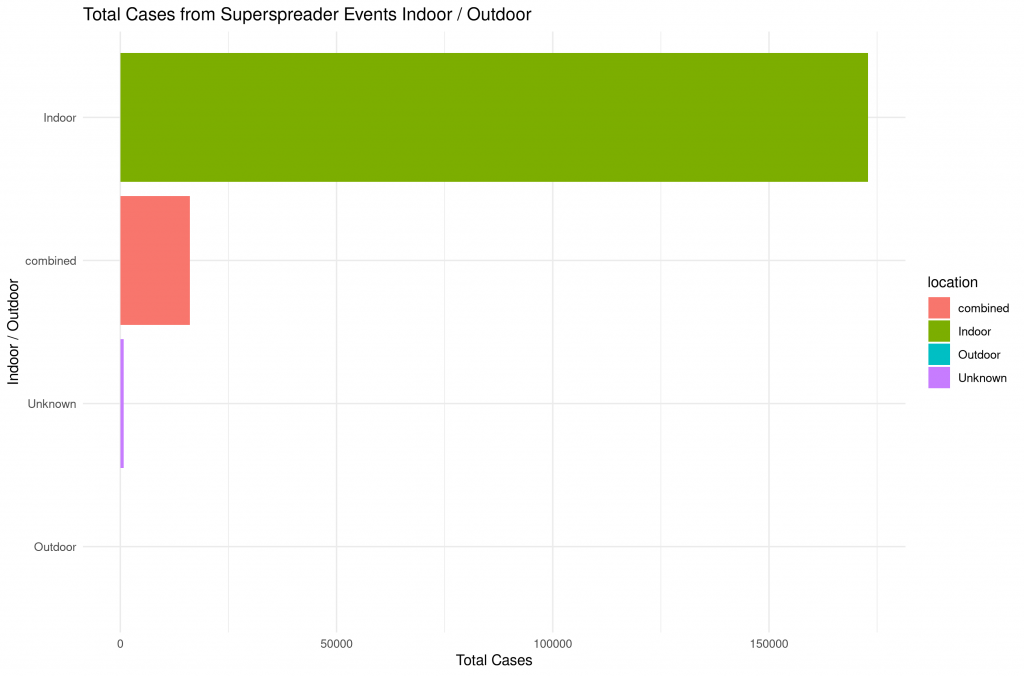
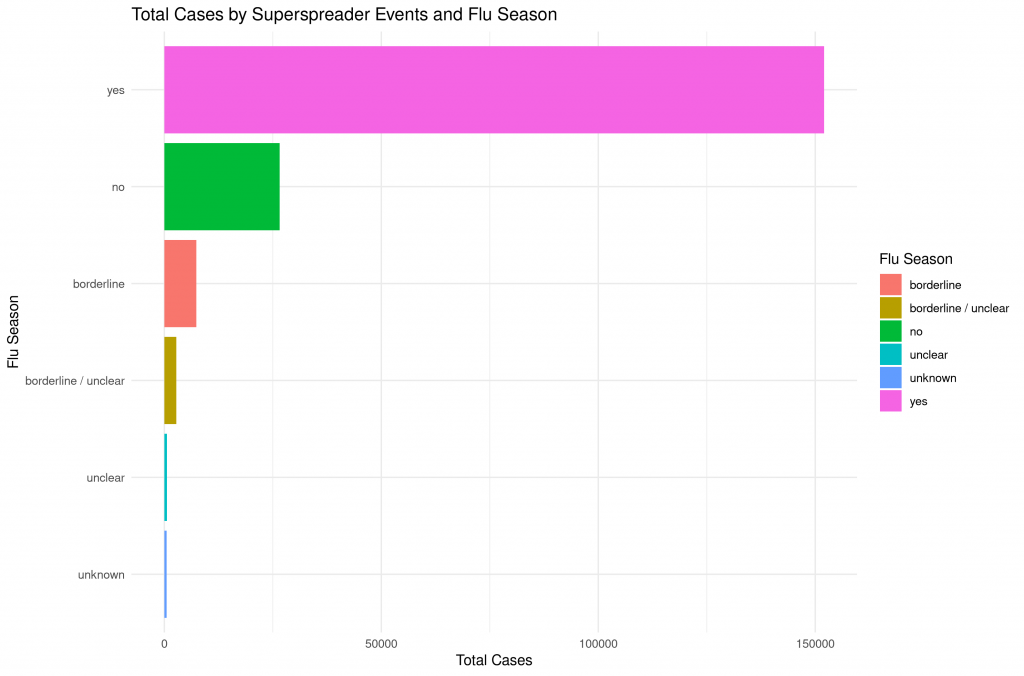
Putting the pieces together, the following picture emerges: Superspreading events play a significant role in driving the pandemic. We may be able to prevent some of these with social distancing, but definitely not all. During the following winter months it may be possible that the number of superspreading events in the Northern Hemisphere will rather increase than decrease. If we take all the secondary, tertiary etc infections into account, the prevention of superspreading events might be of great importance.
Superspreading events are surely an extreme, so let’s step back a bit. Here is an estimate of the individual reproduction number for ‘normal’ transmissions from Adam et al. (right panel):

The basic point I want to make holds for all: Individuals vary greatly in their infection potential and it may make sense to try and identify those who are most at risk of spreading the disease. This is exactly what Rodriguez et al. suggest in a preprint titled “Prioritisation of population groups with the most interactions for COVID-19 vaccination can substantially reduce total fatalities“. Based on simulations they find that fatalities could be reduced by up to 70%. Again not too sure about the precise number, but I think the general point is valid. What would that look like in practice?
Different vaccination strategies
A targeting scheme designed to vaccinate spreaders first would look slightly different from one aimed at the most vulnerable. In both cases, we would try and get vaccines quickly to to medical professionals and nursing homes. But what about seniors outside of nursing homes? If we only cared about the total number of cases and fatalities, they would probably move far down the list. Young and healthy men working at meat processing plants would quickly rise the ladder. Children, adolescents and students in general would quickly follow suit.
Prisons are an interesting case. Under the ‘minimize cases’ scheme, prioritizing the prison population is a no-brainer. In a ‘protect the vulnerable’ world, this is much less clear. Inmates are definitely a population at risk. But different sides of the political spectrum will probably disagree strongly whether or not they qualify as vulnerable and are in their position through no fault of their own. I would argue that protecting its prisoners is one of the core principles of a constitutional state, but I can see how someone would rather see their granny vaccinated than the person who killed their neighbor.
So far, we have looked at specific subgroups of people. But let’s wander off on a thought experiment for a while and attempt to vaccinate the individuals most likely to spread the disease regardless of their profession, age etc. The Friendship Paradox offers an interesting way to achieve that.
The Friendship Paradox states that on average, your friends have more friends than you do. The reason is that you are very likely connected to that one person everybody knows. Someone is more likely to appear in your network if they are themselves very sociable. Someone who doesn’t have a lot of contact to other people is also less likely to be in contact with you. This blog has a very nice illustration using characters from Game of Thrones. Here is their illustration of the network of acquaintances in Game of Thrones:

And this is the distribution of the number of contacts of individuals (red) and their first degree contacts (blue):

We can see that in Game of Thrones, as in real life, your contacts are better connected than you are on average. Let’s take this to the real world. In order to identify those most at risk of spreading the virus, we could simply ask individuals to name those who they were in contact with during the last week or so. We would then obtain a list of names and could simply select those that appeared most often in the list.
Of course we couldn’t. This approach is a) a privacy nightmare and b) subject to crazy amounts of weird incentives. People could try to do weird and dangerous things to get themselves nominated. We don’t want lunatics to run around to increase the amount of contacts they had in order to get a vaccine. I honestly don’t know whether there is a sensible way to achieve something similar (tracing business contacts? contact tracing?). But I would certainly find this a very elegant solution that enables us to quickly identify those we need to vaccinate.
Edit: Maybe we can use the cell phone data of the past month or something like that to avoid people changing their behavior in response to the vaccine announcement. But this still seems a bit shaky.
Other considerations
It is possible that a vaccine might not even be very effective at preventing the spread of the virus. For disease transmission, the amount of virus particles you shed when breathing or talking is important. It is in principle conceivable that a vaccine can prevent a virus from spreading in your entire body, but that the virus can still replicate some time in your mucous membrane in your nose and throat. I am not sure how likely this is, but this seems like an extremely important consideration to determine a vaccination strategy. If you know more, please let me know.
Edit: The scope of what policy makers can eventually decide to do will also be limited by public perception. Even if it were the right thing to do – vaccinating a bunch of students who then go on to throw a college party while their grandparents stay locked inside just doesn’t look good.
Conclusion
For most parts, the default of ‘vaccinating those most at risk’ agrees with the alternative of ‘vaccinating the superspreaders’. This is good as it means that we are likely to end up with a sensible vaccination strategy. Where in doubt, I would lean towards vaccinating spreaders first instead of those most vulnerable. Even though this may seam unfair on the individual level I believe it can save lives in the population as whole. In the end, I believe the best protection we can achieve is a low number of cases.
Ideally I would like to see a system where we try to identify the individuals most at risk of becoming superspreaders. But targeting groups that are likely to be in contact with many people seems like a reasonable proxy for most parts. In the end, policy makers will need to find a balance between the protection of essential workers, the protection of those most vulnerable, and the goal of minimizing future transmissions. I very much hope that they do not try to be ‘tough on crime’, but instead look at the numbers and try to save as many lives as possible.
