The UK moved to a first dose first strategy, where they prioritize vaccine uptake over administering second doses. This means that instead of administering the second dose after three weeks, the UK will delay the booster shot to increase the number of people who have been vaccinated at least once. This is probably excellent news. As I’ve written about before, this essentially means we can vaccinate twice as many people in the beginning.
Here is the relevant quote from the UK report:
In the context of the epidemiology of COVID-19 in the UK in late 2020, the JCVI places a high priority on promoting rapid, high levels of vaccine uptake among vulnerable persons.
Therefore, given data indicating high efficacy from the first dose of both Pfizer-BioNTech and AstraZeneca vaccines, the committee advises that delivery of the first dose to as many eligible individuals as possible should be initially prioritised over delivery of a second vaccine dose. This should maximise the short-term impact of the programme. The second dose of the Pfizer-BioNTech vaccine may be given between 3 to 12 weeks following the first dose. The second dose of the AstraZeneca vaccine may be given between 4 to 12 weeks following the first dose.
A large country like the UK adopting this strategy could be a major game-changer, prompting other countries to follow suit.
Who should get a shot and when?
While the first dose first idea is simple, some of the details are quite complex. Whether to use a shot for a first dose or a booster, depends a lot on the vaccine and who could get it.
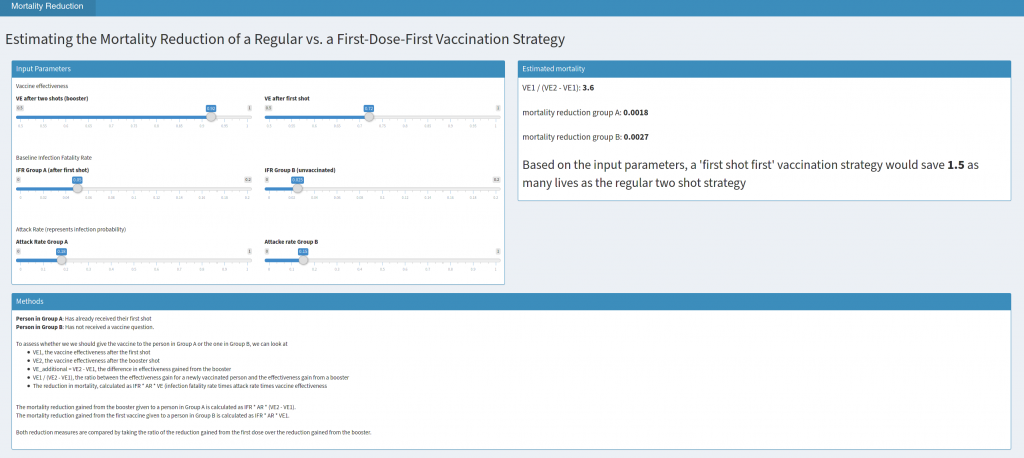
Let’s start by assuming that all people are equally at risk. Then, you should prioritize first doses, if the gain in protection (vaccine effectiveness) from zero to one shot is larger than from one to two shots. Let’s call the vaccine effectiveness (VE) after the first shot VE1 and after the booster VE2. If VE1 > (VE2 – VE1) (or alternatively, if VE1 / (VE2 – VE1) > 1), we should prioritize first doses over boosters. Note that this must always be true if VE1 > 1, since VE2 cannot exceed 1.
This story gets more complicated if we take into account that the two people we could vaccinate may have different characteristics. They could run a different risk of getting Covid-19 (we call that attack rate, AR) and they could have a different risk of dying from the disease once they have it (the infection fatality rate, IFR).
Taking mortality and risk into account
We can calculate the mortality reduction from a initial dose or booster as reduction = VE * AR * IFR. To see whether it is better to give the booster to grandma or to give the first dose to the healthy person working in an exposed work place, we can plug in different values for the expected AR and IFR (Note that for grandma, this is the AR and IFR after the first dose, while for the young worker, it is the IFR and AR before any vaccination).
To get a better intuition for this, I wrote a small app that lets you plug in different values to get an estimate for which strategy would prevent more deaths. When playing around with the inputs, you will see that this simple calculation suggests that prioritizing first doses makes sense in a lot of circumstances, but probably not in all. Still I believe that the UK move was the right one and can possibly a lot of lives.